Methods | Results | The Theory | My Comments | Our Future Project
Albert HB, Sorensen JS, et al. Antibiotic Treatment in Patients with Chronic Low Back Pain and Vertebral Bone Edema (Modic Type I Changes):a Double-Blind Randomized Clinical Controlled Trial of Efficacy. Eur Spine J 2013;22:697-707
In 2013, Albert et al. startled the world of spine research by publishing the results of a double-blind randomized placebo-controlled trial (the highest quality of research there is) which indicated that a simple course of antibiotics was highly effective at reducing chronic back and leg pain in a group of patients who had failed operative care and/or conservative care (a tough group of patients to treat). I agree with his recommendation that patients with disc herniation and Modic change type I at the same level, and who have failed conservative/operative care, may consider a 100-day course of antibiotic therapy in hopes of getting rid of that pain.
Methods:
Only patients who had MRI-confirmed disc herniation, Modic type I change at the same level, and had failed at least six months of conservative care or operative care (discectomy) were enrolled into the study, at which time a new MRI was performed to confirm the volume of Modic type I change. By computer assignment, qualifying patients were given either the real antibiotics (amocicillin-clavulanate Bioclavid™, which is an antibiotic that has low anti-inflammatory properties and does not penetrate the disc) or a fake antibiotic (placebo made of calcium carbonate, but looked identical to the real thing) and asked to take these for 100 days (they were given a medication diary to ensure they complied), which is a time-period commonly employed on patients with confirmed discitis. 90 patients started the real antibiotics and 72 started the placebos. (The randomization was actually a little more complicated, but this accurate and is good enough for our purposes). They were discouraged from doing any other type of treatment or even consultations with medical specialists for the next year; however, they were allowed to continue taking whatever anti-inflammatory/pain medication they were taking prior to the study. Although they used some strange and uncommon outcome assessment tools, they did include the Roland-Morris (a disease specific disability tool) and a simple 0-10 numeric rating scale for back and leg pain. Blood serum from the patients was also taken before the start of the study and at the one-year time-point.
RESULTS
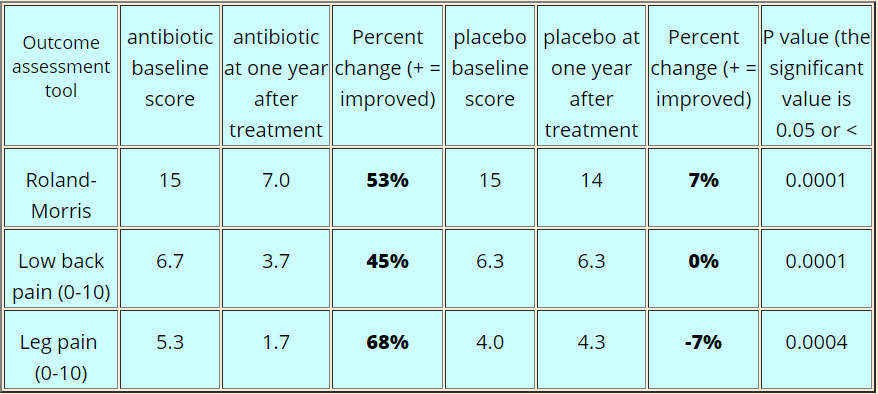
Of the 160 patients entered the study, 144 (88.9%) completed follow-up that one year, which included a repeat MRI. Patients in the antibiotic group achieved higher improvement on all outcome measures as compared to the placebo group (see table below), this included leg pain.
One weird thing was that this improvement did not start for most patients until 6-8 weeks after the start of the real antibiotics – that's a long time.
The volume of Modic type I change also decreased in antibiotic group versus placebo group; however, the placebo group just happened to have more patients with small volume of Modic change at the start of the study, so I'm not impressed and this result should be definitely taken with a grain of salt.
23% of patients in the antibiotic group did consult a medical specialist (we don't know what type of treatment they got); however, 42% of the placebo group sought extra help from medical specialists. Therefore, the improvement in antibiotic group cannot be attributed to extra help from a medical specialist.
Conclusions
The investigators concluded that antibiotic therapy should be considered for patients who have failed conservative or operative care for chronic back/leg pain, but only if they have MRI findings for disc herniation and Modic type I change.
THE THEORY
AAlbert's postulates that common skin bacteria can enter the bloodstream (through activities such as brushing and/or flossing your teeth) and then entered the disc (via its blood supply), herniation (via the new blood vessel growth within that herniation), and/or the annular tear (via new blood vessel in growth).
Most of this bacteria seems to be anaerobic gram-positive, which loves and thrives in a low oxygen environment, such as the inside of the disc and/or in a herniation fragment.
Once bacteria (especially one called p. Acnes, which is the same one that causes acne) take up residency inside the disc or herniation, they secrete, as part of their normal metabolism, an acid (propionic acid) as well as tumor necrosis factor alpha (an evil proinflammatory mediator [a fire starter])
The acid and TNF-a then diffuse from the disc into the vertebral endplates and cause destruction of bone and marrow which in turn starts a general inflammatory process. This inflammatory process sets-off the pain-carrying nerve fiber in the vertebral endplate and causes low back pain, as well as endplate changes (i.e., tyep I Modic changes).
What about the leg pain? How could the bugs cause that?
The authors theorized that the propionic acid and tumor necrosis factor alpha, generated by the bacteria, may have leaked out of the disc onto the nerve roots which in turn caused the patient's sciatica. OR the leg pain was simply a "referred pain" coming from the disc [same thing that occurs when someone gets a heart attack and they get pain down their left arm – that left arm pain is a referred pain].
The antibiotics simply kill off the bacteria which stops the release of propionic acid and tumor necrosis factor alpha, which slowly stops the cause of the pain (irritation of the nerves in the endplate/vertebra).
MY COMMENTS
This theory of bacteria getting into the disc herniation is not new and has been around since the early 2000s. Until this study, it was pretty much laid to rest because of a 2006 study where researchers demonstrated that under super-sterile conditions (they took the cultures and plated them right in the operating room), no anaerobic bugs were found. These findings seem to indicate that all these bacteria found in disc herniations were coming from operating room wound and/or air contamination. So I was incredibly surprised to learn about this powerful new study which demonstrated that antibiotics significantly reduced the back and leg pain of patients who had failed surgery and/or conservative care. These findings have definitely renewed interest in the possibility that a bacterial infection is in fact involved in some patients width chronic back pain and/or sciatica.
There are a few problems, however, which I have e-mailed the author about but have yet to get a response (if I don't soon, I will officially write them up and send them to the editor of the Journal).
STUDY PROBLEMS
Since the patients were allowed to take anti-inflammatories and other medication while the study was going on, we need to make sure that there was no difference between the two groups with regard to usage. For example, what if the patient's in antibiotic group were taking more anti-inflammatories/other medications as compared to patients in the placebo group-- that would not be good.
Did the blood serum test results demonstrate signs of bacteria? They can test for Lipid S (a marker on anaerobic bacteria), which could have told us if bacteria were present in these patients – that's the biggest problem with this study is that we don't know whether or not bacteria were even present in these patients.
Albert mentioned in the article that not all of the patient's completed the course of antibiotics and placebo, but he did not tell us if the noncompliant patients were the same in number between the groups.
Other than that, this was a very well designed study. I agree with Albert's recommendations for patients who have failed conservative care/surgery and have a history of symptomatic disc herniation with Modic type I change at the same level, to consider undergoing a 100 day course of antibiotic therapy.
FUTURE RESEARCH
We have decided to conduct a study here at the Steadman Philipon Research Institute to see if bacteria are really infecting the disc via the circulation--we believe that the bacteria found in HNP material is coming from the surgical incision, not the general circulation.
More specifically, we are randomizing a group of patients undergoing microdiscectomy into either the traditional antiseptic procedure group and a group that will get an extra cleaning of the wound after dissection down to the lamina. Then, as others have done, we will biopsy the disc herniation fragment and compare all the results. We theorized that by super cleaning the wound, the number of bacteria found in the herniated fragment will be virtually nonexistent. I just got it through our IRB, so the results should be quite exciting.
