THE DISC BULGE
The Research | MRI Appearance | Potentially Pain Causing |
*I strongly recommend that you read over the Disc Anatomy Page and MRI Page before reading through this section on disc bulges, for I am going to assume that you are able to look at an axial view of the disc (both on cartoon and MRI) and have at least some understanding of what you are looking at.
Of all the e-mail questions that I receive, one of the most common is, "What is a disc bulge and can it cause pain?"
Although the answer to the first part of the question is easy, (see figure 1) the answer to the second part is much more difficult and not nearly as black-and-white as many doctors would have you believe.
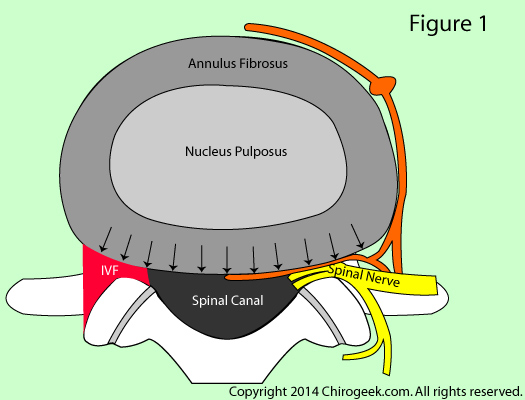 The term "disc bulge" means that the entire backside of the disc is "bulging" backwards. It differs from a disc herniation in that it is a general outpouching of the entire backside of the disc, where herniation is a localized, focal, much smaller outpouching of the back of the disc. To make things a little more complicated, sometimes you can have a focal disc herniation superimposed upon a general bulging!
The term "disc bulge" means that the entire backside of the disc is "bulging" backwards. It differs from a disc herniation in that it is a general outpouching of the entire backside of the disc, where herniation is a localized, focal, much smaller outpouching of the back of the disc. To make things a little more complicated, sometimes you can have a focal disc herniation superimposed upon a general bulging!
Figure 1 is an axial anatomical view through the L4 disc of a motion segment that is significantly bulging posteriorly (arrows).
Note that the bulge is of sufficient magnitude to narrow the spinal canal and neuroforamina (aka: intervertebral foramina or IVF). For comparison, here is a normal looking disc made from the same cartoon.
This patient, however, is probably not experiencing any disc-related pain because the annulus is still intact (i.e., no annular tears have developed) and corralling the nucleus.
You see, in order to know if the disc bulge is causing your chronic pain, we need to know whether or not that bulge is hiding an annular tear; specifically, an annular tear that is large enough to invade the posterior or posterolateral one third of the annulus. Recall from the Disc Anatomy Page that those regions of the annulus contain all of the pain-carrying nerve fibers. *In order to get a visual idea of the disc innervation, have a peek at this link: (Disc Sinuvertebral Nerves)
So how do we go about checking to see if the disc bulge is hiding an annular tear? Unfortunately, this is where the problem lies, for there is no non-invasive (injury-free) way to check a disc bulge for annular tearing.
Although you might luck out and see indications of an annular tear on MRI (about 14% of tears will show up as a high intensity zone {see below}), [1,18] these disc lesions are completely invisible on radiograph (x-rays) and computed tomography (CT).
Therefore, we are stuck with provocative discography as the gold standard for diagnosing annular tears which is a potentially deleterious (harmful) procedure that may result in post-procedure degeneration, annular tear, and even disc herniation.
There is, however, another relatively non-invasive method that may be employed to rule out the disc as a pain generator. This method involves working through a complex diagnostic algorithm which is too complicated to described here.
Disc Bulge: The Research
To confuse things even further, disc bulges are extremely common in pain-free middle age folks! For example, in a landmark study published in the famed New England Journal of Medicine, Jensen et al. [1] reported the MRI results of 98 middle age volunteers who had never had low back pain. Surprisingly, they discovered that 52% of them had at least one disc bulge in the lumbar spine. [1]
Well, if that is true, then you might theorized that people with low back pain must have an even higher prevalence (frequency) of these disc bulges. Although your logic is sound, it is not true!
In another historic MRI investigation, Albert et al. (2011) published the results of their study that analyzed over 4000 MRI scans from low back pain patients entering a spine clinic. After analyzing all the data, they discovered that 65.2% of the patients had at least one disc bulge in the lumbar spine. [18]
Therefore, although asymptomatic volunteers had a slightly higher prevalence of disc bulge (52%), that number was not statistically different from the prevalence of disc bulge in low back pain patients (65.2%). (p>0.05)
Disc Bulge: the MRI Appearance
 Remember I said that answering the first part of the question ("what is a disc bulge....") is easy? Well it is. Let's take a look at some MRIs.
Remember I said that answering the first part of the question ("what is a disc bulge....") is easy? Well it is. Let's take a look at some MRIs.
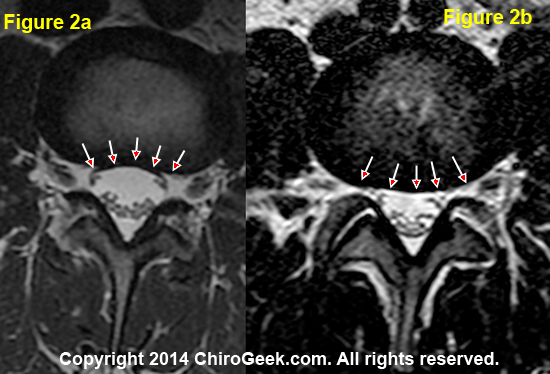
Figure 2a is a normal looking T2-weighted axial MRI image of an L3 disc from a middle-aged male. Note the concave posterior appearance of the disc (arrows).
Figure 2b, which is also a T2-weighted axial image of an L3 disc in another middle-aged male, clearly demonstrates that the posterior disc has lost its normal concavity and is "bulging out" in a smooth and general fashion.
That's it! It's really not so difficult to see a bulging disc.
*In reality, things are a little more complicated because some disc shapes are not always concave at the posterior—especially at L4 and L5. In these situations, you simply look at whether or not the disc is bulging into the neural foramina and spinal canal.
Disc Bulge versus Disc Herniation
 Although I'm sure you are all pros at picking out a disc herniation, I better cover this sub-topic quickly just to make sure.
Although I'm sure you are all pros at picking out a disc herniation, I better cover this sub-topic quickly just to make sure.
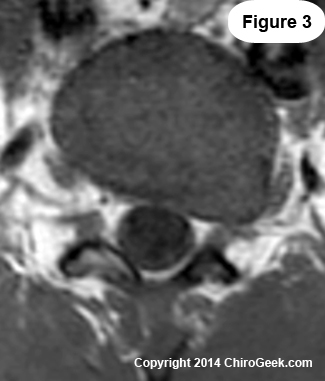
Compare figure 3 to figure 2b. What do you see? Is this a bulge?
The back of the disc is bulging out, but this time it is not a smooth general bulging of the entire posterior disc. This time, we have a focal or very isolated region of bulging in and outside of the leftneural foramen (remember, these images are reversed with regard to sidedness).
Any time you see a focal disc bulging, then you have a condition called a disc herniation (aka: disc protrusion, disc prolapse, or "slipped disc").
Furthermore, if you see a herniation this large (this one is compressing the exiting nerve root), then the chance of it being a false positive (not causing pain) is very slim—approximately 1% of the time. [1]
If you still can't see the herniation, go to the forthcoming link in which I have outlined the contour of the disc, posterior arch, and herniation (in red). (Figure 3 Markup)
Disc Bulge: MRI Signs of Pain
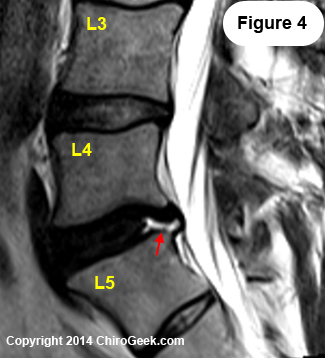 As mentioned above, the MRI images of about 14% of patients with chronic low back pain will display an area of bright white signal in the posterior periphery of the disc on T2-weighted MRI. [1,18] This imaging finding is known as an HIZ. (figure 4, red arrow)
As mentioned above, the MRI images of about 14% of patients with chronic low back pain will display an area of bright white signal in the posterior periphery of the disc on T2-weighted MRI. [1,18] This imaging finding is known as an HIZ. (figure 4, red arrow)
Pathoanatomically speaking, an HIZ represents a region of vascularised granulation tissue (the precursor to scar tissue) [21] that is found within the annular tear. Why is it there? It is an attempt by the body to heal the tear.
Figure 4 demonstrates a massive HIZ in the posterior annulus of the L4 disc (red arrow) as viewed on this T2-weighted MRI image. This 35-year-old male suffered from debilitating low back pain and was contemplating interbody fusion.
The reason annular tears show up bright white on T2-weighted MRI imaging (it must be just as white as the cerebrospinal fluid in order to be officially called a HIZ) is because the vascularised granulation tissue contains a lot of fluid and blood, and as we have learned, fluid and blood show up bright white on the T2 MRI.
If you happen to see one of these in your disc, and you have chronic low back pain that has yet to be diagnosed (i.e., no stenosis, spondylolisthesis, spondylolysis, or disc herniation), then the chances are pretty good that your disc is in fact the source of the low back pain. [20,22,23]
In 1996, Schellhas et al. performed discography on 100 discs of patients with chronic low back pain, all in whom had MRI evidence of HIZ. Discography results found a high correlation between the presence of HIZ and positive discography (i.e., the patient experienced concordant pain during the procedure). During the same study, 67 discs from low back pain patients without HIZ also underwent discography. This time, 97% of those discs tested negative on discography (i.e., either no pain, or non-concordant pain was elicited). These findings led the authors to conclude, "In patients with symptomatic low back pain, the high-intensity zone is a reliable marker of [a] painful outer annular disruption." [20]
References:
#1) Jensen MC, et al. “MRI imaging of the lumbar spine in people without back pain.” N Engl J Med – 1994; 331:369-373
#2) Boden SD et al. “Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects: A prospective investigation.” J Bone Joint Surg Am 1990; 72A:403-408
#3) Weishaupt D et al. “MRI of the lumbar spine: Prevalence of intervertebral disc extrusion and sequestration, nerve root compression and plate abnormalities, and osteoarthritis of the fact joints in Asymptomatic Volunteers.” Radiology – 1998; 209:661-666
#4) Boos N, et al. “1995 Volvo Award in clinical science: The diagnostic accuracy of MRI, work perception, and psychosocial factors in identifying symptomatic disc herniations.” Spine – 1995; 20:2613-2625
#5) Schwarzer AC, Aprill CN, Derby R, Bogduk N, Kine G. “ The prevalence and clinical features of Internal Disc Disruption in patients with Chronic Low Back Pain. ” Spine 1995; 20(17):1878-1883
#6) Crock HV. "Internal disc disruption: A challenge to disc prolapse fifty years on." Spine 1986 ;11:650-3
#7) Milette PC, et al. “Radiating Pain to the Lower Extremities Caused by Lumbar Disk Rupture without Spinal Nerve Root Involvement.” AJNR Am J Neuroradiol 1995; 16:1605-1613
#8) Ohnmeiss DD, et al "Degree of disc disruption and lower extremity pain" Spine - 1997; 22(14):1600-1665
#9) Ohnmeiss DD, et al. "Relationship of pain drawings to invasive tests assessing intervertebral disc pathology." Eur Spine J 1999; 8(2):126-131
#10) Ohnmeiss DD, et al. "Relation between pain location and disc pathology: a study of pain drawings and CT/discography." Clin J. Pain 1999; 15(3):210-7
#11) Marshall LL, et al. "Chemical radiculitis: A clinical, physiological and immunological study." Clin Orthop - 1977:129:61-7
#12) Marshall LL, et al. “Chemical irritation of nerve root in disc prolapse.” Lancet 1973; 2:320
#13) Olmarker K et al. “Autologous nucleus pulposus induces neurophysiologic and histologic changes in porcine cauda equina nerve roots [see comments] Spine 1993; 18:1425-32
#14) Olmarker K, Larsson K. “Tumor necrosis factor alpha, and nucleus-pulposus-induced nerve root injury.” Spine 1998; 23:2538-2544
#15) Kayama S, Olmarker K, et al. “Incision of the anulus fibrosus induces nerve root morphologic, vascular, and functional changes: An experimental study.” Spine 1996;21:2539-43
#16) Olmarker K, Brisby H, Rydevik B, et al. “The effects of normal, frozen, and hyaluronidase-digested nucleus pulposus on nerve root structure and function.” Spine 1997; 22:471-5discussion 476
#17) Byrod G, Reydevik B, Olmarker K, et al. “Acute increase in endoneural vascular permeability induced by epidural application of nucleus pulposus on spinal nerve roots. Manuscript [550]
#18) Albert HB, Briggs AM, Kent P, et al. The prevalence of MRI-define spinal pathoanatomies and their association with Modic changes in individual seeking care for low back pain. Eur Spine J 2011;20:1355-1362.
#19) Hanna H, Tommy H. HIZ's relation to axial load and low back pain: investigated with axial loaded MRI and pressure controlled discography. Eur Spine J 2012;22:734-739.
#20) Schellhas KP, Pollei SR, Gundry CR, et al. Lumbar disc high-intensity zone: correlation of magnetic resonance imaging and discography. Spine 1996;21:79-86.
#21) Peng B, Hou S, Wu W, et al. The pathogenesis and clinical significance of a high-intensity zone of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J 2006; 15:583-587.
#22) Chen JY, Ding Y, Lv RY, et al. Correlation between MR imaging and discography with provocative concordant pain in patients with low back pain. Clin J Pain 2011;27:125-130.
#23) Kang CH, Kim YH, Lee SH, Derby R, et al. Can magnetic resonance imaging accurately predict concordant pain provocation during provocative disc injection? Skeletal Radiol 2009;38:877-885.
