microdiscectomy
The Procedure |Proper Candidate | Surgery Timing | Chance of Success | Open Microdiscectomy |History of Discectomy | Surgery Position | Picking vs. Sequestrectomy | Endoscopic Discectomy |Laser Discectomy
When a lumbar disc herniation occurs, it usually happens in the posterolateral region of the disc, an area that does not have the extra reinforcement of the posterior longitudinal ligament. If the herniation is large enough, it will contact or even compress the adjacent traversing nerve root which is typically still inside the thecal sac (at L5/S1 it may have already budded out of the thecal sac).
In some, but not all, patients, the contacts/compression of the disc herniation against the nerve root will result in an inflammation of that nerve root which in turn causes radicular pain, or better known as sciatica, which can be described as a terrible burning, numbing, and/or electrical -like pain that shoots down the lower extremity. {If you have no idea what I'm talking about, should probably go to the disc herniation page and learn about that before you come here.}
For patients who have failed all conservative care (physical therapy, chiropractic care, acupuncture, and/or medication), the gold standard treatment (undisputed king) for eliminating/reducing the sciatica is a surgery called a microdiscectomy.
These days there are several types of discectomy available; however, on this page I will describe the time-tested gold standard, which is called microdiscectomy.
How does it work? In a nutshell, the surgeon will carefully enter the epidural space from the backside, retract the thecal sac out of the way, and then remove that pesky disc herniation. By removing the disc herniation, it eliminates the compression of the nerve root and eliminates inflammatory cytokines which are leaking onto the nerve root and at least in part causing the inflammation.
Now there are many good YouTube videos on this procedure, but here are five overhead pictures that described the basics of what's going on.
OPEN DISCECTOMY PROCEDURE:
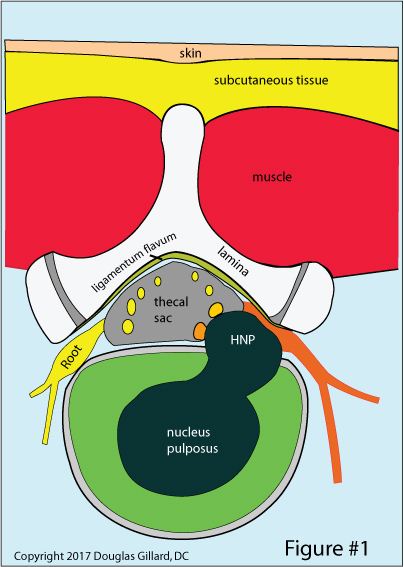
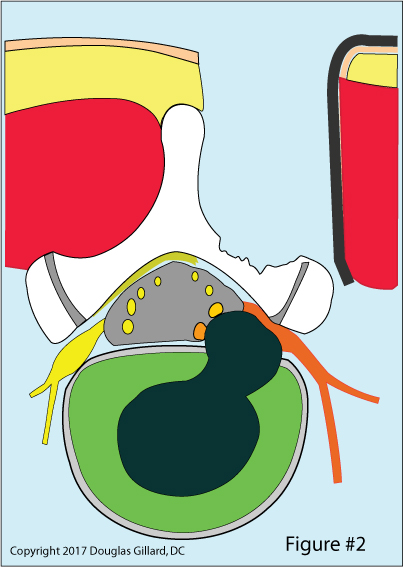
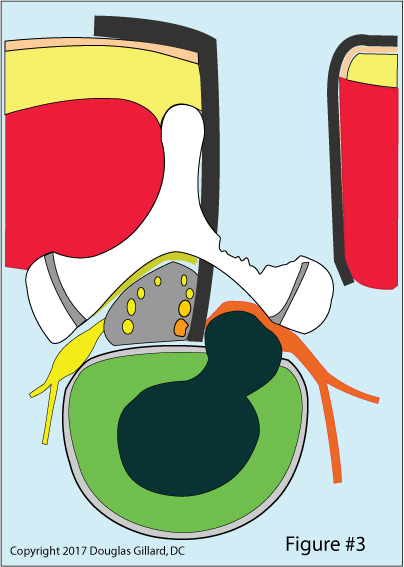
Figure #3: Next, the bony lamina is partially removed (laminotomy) at L4 and L5, which reveals the final guardian of the epidural space, the ligamentum flavum. It too is removed. Next another retractor is used to push the thecal sac and traversing nerve root medially (out of the way). finally, the HNP is revealed.
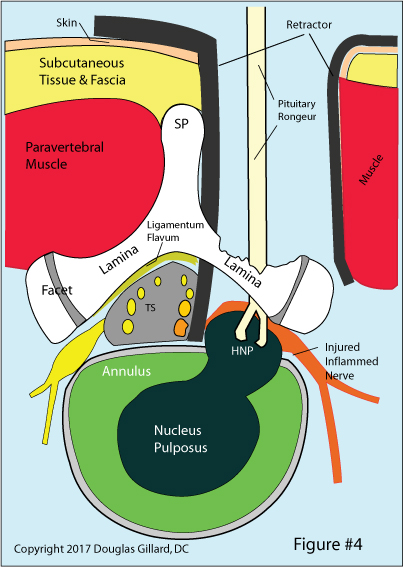
Figure #4: The rongeur has been carefully inserted through the surgical incision, between the laminae, and has grabbed onto the herniated nucleus pulposus material.
Next, the surgeon pulls the rongeur and herniation back out of the incision. Most likely, he or she will need to go back in several more times, in order get all of this herniated nucleus pulposus out.
WHAT MAKES A GOOD CANDIDATE FOR DISCECTOMY?:
Please remember that the following information, as well as all the information on this website, is strictly for educational purposes. Never act on any of this information without getting a second opinion from a spine care professional.
Also please remember that I do offer a GoToMeeting Consultation Service (I call this a coaching service) in which you and I will go over your MRI/CT images, slice-by-slice, and then formulate a plan of action based on the current medical evidence. If you're interested, please email me or visit my Coaching Service Page.
Who is a proper candidate for discectomy?
A proper candidate can be defined as the patient who has (1) imaging evidence (MRI, CT myelography, and/or CT discography) of a herniation that matches neurological findings on exam; (2) nerve root tension signs (i.e., a positive straight leg raise or reverse straight leg raise test); and (3) subjective complaints that match examination findings and subjective complaints.
Who are mandatory candidates for discectomy? the short answer is this: patients with (1) cauda equina syndrome; (2) severe progressive neurological findings; and//or (3) severe intractable pain. let's talk about them:
Sometimes the disc herniation is so large that it compresses the nerves that control the bowel and bladder. More specifically, the S3 nerve root. if the compression is severe enough, it can cause dysfunction of the S3 nerve root which can present as the classic signs of cauda equina syndrome.
Cauda Equina Syndrome:
Cauda equina syndrome (CES) can be a medical emergency. It occurs when "something" damages the S3 nerve root to the point of causing its dysfunction. Once damaged, the internal and extern urethral sphincters (the valves that keep urine inside your bladder) start to lose function which results in symptoms. If severe, CES can result in a nonfunctional bladder (neurogenic bladder) which can only be emptied by the use of a catheter.
There are two types of cauda equina syndrome: incomplete cauda equina syndrome and complete cauda equina syndrome. The subject is now getting beyond the scope of this webpage, but in a nutshell incomplete cauda equina syndrome means that the S3 nerve root is been damaged right now. This is the medical emergency. If there is a compressive lesion, like a disc herniation, or a bleeding into the epidural space or anything else that damages the S3 nerve root, emergency surgery (within 24 hours) is necessitated in attempts to save the bladder. Signs of incomplete cauda equina syndrome include urinary hesitancy and perineal dysesthesia (numbness/burning of the bike-seat area).
Other Recommendations for Discectomy:
The American Academy of Orthopedic Surgeons and Alf Nachemson – who was the number one spine researcher in the world (18) -- recommends the following conditions be met before decompressive surgery is offered:
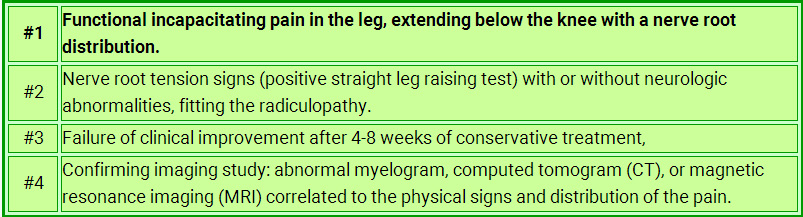
SURGERY TIMING: When Is It Time?
The Short answer is that you should only fool around with true disc herniation-induced sciatica for three or four months--if it ain't better by then, and you meet the above criteria, then you should seriously consider having open microdiscectomy surgery.
The forthcoming chart demonstrates what the research says about the timing of discectomy. As you can see, the average recommendation is 4.2 months. Also, remember that really good spine surgeons are not easy to see. It could take two or even three months to get in to see one, so keep that in mind when you're going through your conservative care program.
THE RESEARCH: What Are My Chances for Success Following Discectomies?
What does the research say about the chances of having a successful open/microdiscectomy? While there are hundreds if not thousands of investigations describing the efficacy and outcomes of discectomy, arguably the best research study on the subject to date is the Maine Study [1]:
In 2005, Atlas et al. published the results of their 10 year outcome study, which followed 507 patients in whom suffered disc herniation-induced back pain and sciatica. At the 10 year time point, 84% of these patients were available for the follow-up, which makes this a high-quality investigation, and is quite a difficult feat to pull off.
At the beginning of the study, approximately 1/2 of the patients were allocated into conservative care, while the remaining 1/2 were allocated to discectomy surgery (this group actually had more severe symptomatology). At the 10 year time point, the patients who had surgery were significantly better (p=0.002) than the patients who did not have back surgery. Specifically, 56% of the surgical patients reported that their low back and leg pain were much better or completely gone. However, only 40% of the nonsurgical patients reported such improvement (P = 0.006). Patient satisfaction was also significantly better in the surgery group: 71% of the surgery patients were satisfied with their outcome, while only 56% of the nonsurgical patients were satisfied (P = 0.002). However, despite the favorable subjective performance of discectomy, both groups were statistically equal with regard to the ability to work and disability status at 10 years.
Note that most people do not get 100% better: it doesn't matter whether you have discectomy or just go with conservative care, more likely than not you're still going to end up with a significant disability if you have real disc-herniation related back and leg pain.
Which Type of Discectomy Do I Get?
The short answer is this: it all depends on your unique situation. Typically, open discectomy is the gold standard treatment for a straightforward paracentral disc herniation. However, sometimes endoscopic techniques are useful, especially if the disc herniation is located in the far lateral zone.
What are the available choices of discectomy?the major discectomy techniques include open microdiscectomy, laser discectomy, endoscopic discectomy, percutaneous discectomy, nucleoplasty, and the disc volume reduction techniques. I am not going to get into all of those here, but have covered many of them on separate pages within my website, ChiroGeek.com.
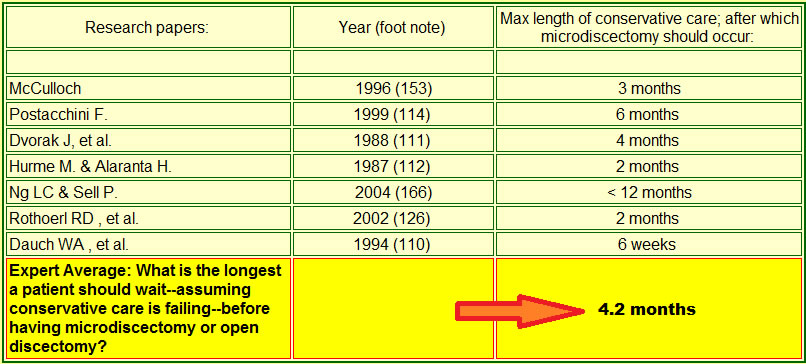
The History of Discectomy
As all astute physicians know, 1934 was a good year. This is because the timeless mystery of sciatica (which has plagued mankind long before the days of Hippocrates (300 B.C.)) was finally uncovered and the open discectomy was born.
The procedure was very crude at first in the beginning: they used to do a complete laminectomy (completely remove the lamina on both sides); flavectomy (completely remove the ligamentum flavum on both sides) and finish by, believe it or not, cutting right through the CSF-containing thecal sac (transdural approach)! They didn't retract the thecal sac (push it) out of the way like they do these days. Nope! They went right through the thecal sac in order to access the herniation (transdural approach)--indeed a very scary surgery. The amount of scar tissue that must have been generated is unthinkable!
Subsequent modifications, however, created the very successful procedure for the treatment disc herniation-induced sciatica [1, 13] that we have today. Specifically, these modifications, all of which significantly reduce the amount of epidural fibrosis, include the following:
- Retraction of the thecal sac, and/or nerve root, out of the way.
- The use of laminotomy in place of laminectomy [73]
- A minimal flavectomy (don't take out as much of ligamentum flavum as they used to)
- the use of high-powered magnification via magnification glasses or loupes
More Detailed History
Grafton Love, a surgeon at the Mayo Clinic, put his twist on the open discectomy technique in 1939, using what he called a "key hole" laminotomy to access the epidural space--microdiscectomy was born [73].
In 1977, Yasargil [24] and Caspar [25] independently described the addition of a powerful operating microscope to the open discectomy procedure that resulted in a much more minimally invasive procedure. That is, the microscope greatly increased the physician's vision, which in turn resulted in smaller and cleaner dissections down to the disc herniation. Arguably, this precision results in less soft tissue damage and less postsurgical scarring (epidural fibrosis and perineural fibrosis), which in turn yields better patient outcomes when compared to traditional open discectomy. And that superiority is just what the first outcome study on microdiscectomy demonstrated [5]. Current studies, however, are not so persuasive (see below).
This page would be incomplete without a historical discussion leading up to that landmark discovery that a herniated intervertebral disc could result in lower back pain as well as terrible radiating lower extremity pain (sciatica).
No doubt humans have toiled with back pain and sciatica since they evolved to an upright posture, which in turn pressurized the intervertebral disks. The first written reports of back pain and sciatica surfaced in the ancient medical text The Edwin Smith Surgical Papyrus, which was ostensibly written around 1550 BC [10].
The famed German pathologist, Hubert von Luschka, was the first to thoroughly describe the different classes of disc herniation back in the 19th-century. Notwithstanding his thorough descriptions (which were gleaned from cadaver dissection), not only did he fail to clinically associate these herniations with back pain and leg pain, he also erroneously described these disc protrusions as cartilaginous tumors of the disc.
In December 1908, German surgeon Fedor Krause performed the first successful discectomies/laminectomy on a patient who suffered from severe sciatica that had progressed into cauda equina syndrome [90]. However, despite the resolution of sciatica and urinary incontinence, he still didn't put two-and-two together and opined the patient's incontinence was secondary to a discal enchondroma (cartilage tumor)—in reality, the large mass he removed from the disc was a large disc herniation.
Professor Walter E. Dandy, a neurosurgeon at John Hopkins, was almost there when he published a revolutionary hypothesis that these masses in the posterolateral region of some intervertebral discs were not tumors but in fact were made of discal tissue [26]. Furthermore, he postulated that these masses could in fact produce patient sciatica by compressing the adjacent nerve roots. He even proclaimed that by their removal, the patient's pain could be cured. Unfortunately, little attention was paid to his publication because he continued to call these disc protrusions tumors-- that was his only mistake. Dandy, however, is often credited with performing the first surgical treatment for a disc herniation that resulted in cauda equina syndrome in two patients [30].
The Famous Mixter Barr: In 1934, American neurosurgeon William J. Mixter and orthopedic spine surgeon Joseph S. Barr, rocked the medical world by proclaiming that these supposed enchondroma of the disc were nothing more than herniations of disc material (the nucleus pulposus) from within the same disc–herniations were not tumors. These Massachusetts general doctors also explained how compression of the nerve roots could create the symptom of sciatica as well as back pain.
More specifically, they stated the following:
"We conclude from this study: that a herniation of the nucleus pulposus into the spinal canal, or as we prefer to call it, rupture of the intervertebral disc, is a not uncommon cause of symptoms. That the lesion frequently has been mistaken for cartilaginous neoplasm arising from the intervertebral disc…. That the treatment of this disease is surgical and that the results obtained are very satisfactory if compression has not been too prolonged." So after hundreds of years, the mystery was finally solved.
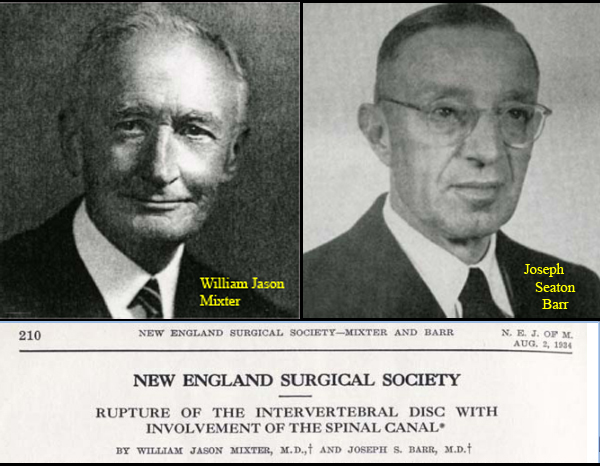
SURGERY POSITION:
In general, there are two types of tables used to perform the discectomy procedures: the Relton-Hall table (which yields a more prone patient position) and the Andrews table (which yields a knee-chest position). *Sometimes these are called frames instead of tables.
So which one is best? The research shows that both tables are about the same and both afford the best possible position for surgery.
How do you know that? The research:
In 2005, Rigamoni et al. [14] published the results of their investigation into which surgical table would afford the best results following micro/open discectomy. More specifically, they wanted to see which table minimized intraoperative bleeding. In general, intraoperative bleeding is a direct result of the magnitude of intra-abdominal pressure, which can be manipulated by placing the patient in different positions during surgery.
In this study a total of 30 patients ready for single level lumbar microdiscectomy had their intra-abdominal pressure measured through a urinary bladder catheter together with airway pressure. Several different positions were tested in the patients, who were randomly assign these positions. the bottom line of the investigation was that there was no statistical difference with regard to the more prone position of the Relton-Hall table, versus the more knee-chest position of the Andrews-type table [14].
There are also other frames commonly used, such as the Jackson frame.
PICKING VS. SEQUESTRECTOMY: To pick, or not to pick. That is the question.
One of the major complications with Discectomy is the dreaded recurrent disc herniations (i.e., the herniation was surgically removed, but it returned again--through the same annular tear). More specifically, the incidence of such reherniations is, depending on the source, between 1 and 11% [23-25].
In order to reduce those percentages, surgeons perform either type of discectomy via two methodologies: to only remove the herniated material that is outside of the confines of the annulus fibrosis (this type of surgery is called a sequestrectomy); or to explore the annular tear (inside the disc) and remove any fragments of nuclear material (I call this camp "the picking technique") that may be lurking about. The latter methodology is the norm.
You see, many surgeons believe that aggressive removal of nuclear fragments within the annulus will prevent further reherniation simply because there will be less nuclear material to herniate.
However, there is scientific research that contradicts this general belief. An especially scientifically strong randomized controlled trial [25] of 84 patients demonstrated that sequestrectomy resulted in fewer reherniation at the one year time point [25]. However, those same researchers found no difference between the two techniques in subsequent investigations at a two-year follow-up [22, 23].
Bottom line: the research says when it comes to open versus microdiscectomy there is really no difference between sequestrectomy and traditional "picking technique."
As a side note, there is a third school of thought that not only performs a sequestrectomy and "picking" of the annular tear, but also uses a special dye to stain the walls of the annular tear for pre-fragment / degenerated tissue, which in turn is removed. There is virtually no research on this form of treatment, so the jury is still out on whether or not it is efficacious.
THE FUTURE? Endoscopic Microdiscectomy:
In hopes of mitigating tissue damage via dissection, surgeons are now using endoscopes to perform and even more minimally invasive form of microdiscectomy. Although the so-called microendoscopic discectomy is a relatively new procedure, it allows for smaller incisions, less tissue trauma, no need for general anesthesia, reduced hospital stays, and reduced cost when compared to open microdiscectomy.
It was Foley and Smith whom more recently reported on the latest innovation of endoscopic discectomy. [31, 32]. This approach is a hybrid between a percutaneous flavor of discectomy and open microdiscectomy. They named this procedure microendoscopic discectomy (MED). More specifically, this procedure uses a K-wire to get down to the lamina on the side of the herniation. Once in its proper position, A series of dilators (METRx-MED system)--the first is very small and the others are added in increasing Order of diameter--are placed over the K-wire, which have the effect to push the paraspinal musculature off the lamina. The working channel of the endoscope is placed over the final dilator and finally the endoscope is attached. Then a standard microdiscectomy is performed which includes a hemi-laminotomy and sometime a medial facetectomy, followed by a removal of part of ligamentum flavum, then retraction of the thecal sac and nerve root--this exposes the disc herniation, which is then removed. If the surgeon so desires, he can attach a standard microscope to the system instead of an endoscope.
One touted strength of this METRx-MED system over minimally invasive endoscopic techniques for disc herniation removal is that it has the capability of addressing bony stenotic conditions, sequestrations, as well as small contained disc herniations. Observational studies have demonstrated the procedures short term efficacy [32] and long-term efficacy [33].
While the jury is still out on the efficacy of endoscopic microdiscectomy, there is some evidence hinting at their superiority to open discectomy and even microdiscectomy. More specifically, in 2002 German investigators Schick et al. published the results of their study that pitted open discectomy against endoscopic discectomy. They were specifically interested in whether or not use of the endoscope mitigated stress/injury to the dura and nerve roots when they are retracted out of the way during discectomy. To accomplish this, they monitored the lumbosacral nerve roots electromyographically during the operations of 15 patients who underwent open discectomy and 15 patients who underwent endoscopic discectomy. The results indicated that the endoscopic technique afforded less nerve root irritation (as confirmed by EMG) when compared to the open procedure [88].
We shall keep an eye on this technique and report any further studies showing its superiority.
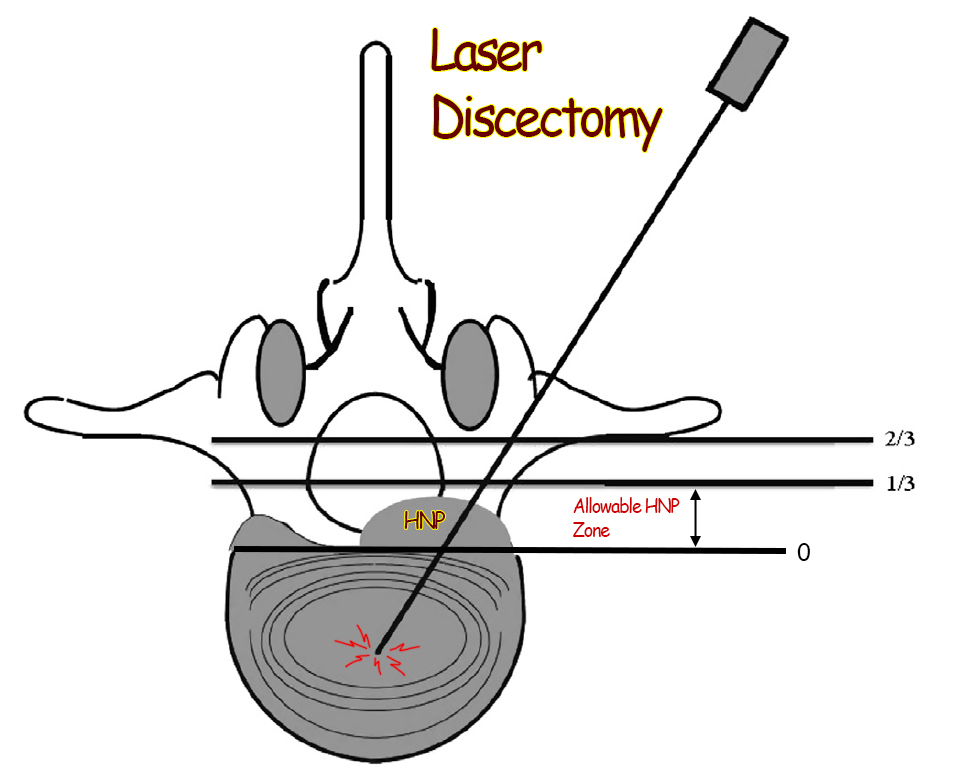
Laser Discectomy/decompression
Some physicians believe that they can treat disc herniations and annular tear via the application of laser energy to the tear and the inner part of the disc (nucleus pulposus). Furthermore, they believe they can remove pain-causing degenerative tissue from the inside of the disc and/or annular tear and decrease the volume of the nucleus which in turn reduces the size of a small herniation, which in turn removes any compression on the adjacent nerve roots.
I just spent four days going over the medical literature database in hopes of finding at least some evidence that would support the use of laser discectomy over conventional discectomy techniques, and I was shocked to find only a single multi-center randomized controlled trial from the Netherlands, which was not well written but nevertheless made it into the number one spine Journal in the world, The Spine Journal.
Bottom line: I now completely understand why insurance companies do not pay for laser discectomy: there is no proof that it works! In this 2015 study, which is one-of-a-kind in the world of laser discectomy, Brouwer et al demonstrated that 44% of the patients who were in the laser discectomy group needed a second surgery within 12 months! A massive failure of the procedure. Please check out my in-depth review of this one-of-a kind randomized control trial on my research Blog.
REFERENCES:
1) Atlas SJ, Keller RB, et al. “long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the main lumbar spine study." Spine 2005; 8:927-935.2) Leonardi M, Boos N. “Disc Herniation and Radiculopathy." In: Boos N, Aebi M, Spinal Disorders: The Fundamentals of Diagnosis and Treatment. Verlag Berlin Heidelberg New York: Springer; 2008.
3) Spengler DM. “Lumbar discectomy. Results with limited disc excision and selective foraminotomy." Spine 1982; 7:604-7.
4) Henriksen L, Schmidt K, Eskesen V, Jantzen E (1996) a controlled study of microsurgical versus standard lumbar discectomy. Br J Neurosurg 10:289-293.
5) Williams RW (1978). "Micro-lumbar discectomy: a conservative surgical approach to the Virgin herniated lumbar disc." Spine 1978; 3:175-182.
6) Ross JS, Robertson JT, et al. “Association between peridural scar and recurrent radicular pain after lumbar discectomy: magnetic resonance evaluation.” Neurosurgery 1996; 38:855-863.
7) Fritsch EW, Heisel J, Rupp S. “the failed back surgical syndrome. Reasons, intraoperative findings, and long-term results: a report of 182 operative treatments." Spine 1996; 21:626-63.
8) Katayama Y, Matsuyama Y, et al. “Comparison of Surgical Outcomes between Macrodiscectomy and Microdiscectomy For Lumbar Disc Herniation: a Prospective Randomized Study With Surgery Performed by the Same Spine Surgeon." J Spinal Discord Tech (2006) 5:344-347.
9) Tullberg T, Isacson J, Weidenhielm L. “Does Microscopic Removal of Lumbar Disc Herniation Lead to Better Results Than the Standard Procedure? Results of one-year randomized study." Spine 1993; 1:24-27.
10) Breasted JH (1930) Edwin Smith Surgical Papyrus, in Facsimile and Hieroglyphic Transliteration and with Translation and Commentary, 2 vols. Chicago: University of Chicago Oriental Publications.
11) Mixter WJ, Barr JS (1934) Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med 211:210-225.
12] Wetzel FT, Hanley Jr. EN. “Spine Surgery: A Practical Atlas. The McGraw-Hill Companies 2002; New York.
13) Henrik Weber, '1982 Volvo Award in Clinical Science' "Lumbar Disc Herniation: A controlled, Prospective Study with Ten Years of Observation." Spine - 1983; 8(2):131-140
14) Rigamoni A, Gemma M, et al. “prone versus knee-chest position for microdiscectomy: a prospective randomized study of intra-abdominal pressure and intraoperative bleeding." Spine 2005; 17:1918-1923.
15) Daniel H Kim, John J Regan. "Endoscopic Spine Surgery and Instrumentation."; Thieme medical publishers: New York 2005
16) Deyo RA (2007). “Back surgery-who needs it?" N Engl J Med; 356:2239-2243.
17) McCulloch JA (1996) focus That issue on lumbar disc herniations: macro-and microdiscectomy. Spine 21:45S-56S.
18) Gibson JN, Waddell G (2007) surgical interventions for lumbar disc prolapse: update Cochrane review. Spine 32:1735-1747.
19) Peul WC, van Houwelingen HC, et al. (2007). “Surgery versus prolonged conservative care for sciatica." N Engl J Med 356:2245-2256.
20) Schmidek HH, Sweet WH, (eds.): Operative neurosurgical techniques. 1st ed., Grune and Stratton, New York, 1982
21) Fager CA: lumbar discectomies; a contrary opinion. Clin Neurosurg 33:419;56, 1986.
22) Katayama Y, Matsuyama Y Yoshihara H, et al. Comparison of surgical outcomes between macrodiscectomy and microdiscectomy for lumbar disc herniations: a prospective randomized study with surgical performance at the same spine surgeon. J Spinal Discord Tech 2006; 19(5): 344-347.
23) Barth M. Diepers M, et al. "Two-year outcome after microdiscectomy versus microscopic sequestrectomy. Part 2. Radiographic evaluation and correlation with clinical outcome." Spine 2008; 33(3): 273-279.
24) Yasargil MG (1977) microsurgical discectomy: a conservative surgical approach to the Virgin herniated lumbar disc. Adv Neurosurg 4:81.
25) Caspar W (1977) a new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. Adv Neurosurg 4:74-80.
26) Dandy WE (1918) Loose Cartilage from the Intervertebral Disc Stimulating Tumor of the Spinal Cord." Arch Surg 68:5-11.
27) Wera GD, Marcus RE, et al. Failure within one year following subtotal lumbar discectomy. J Bone Joint Surg Am 2008; 90:10-15.
28) Isaacs RE. Podichetty V, Fessler RG. microendoscopic discectomy for recurrent disc herniations. Neurosurg Focus 2003; 15(3):E11
29) Thome C, Barth M, et al. Outcome after lumbar sequestrectomy compared with microdiscectomy: a prospective randomized study. Neurosurg Spine 2005; 2(3): 271-278.
30) Dandy WE. Loose cartilage from intervertebral disc simulating tumor of the spinal cord. Arch Surg 1929; 19:660-672.
31) Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg; 1997; 3;301-307.
32) Smith MW, Foley KT. "MED: the first hundred cases." Presented at the Annual Meeting of the Congress of Neurological Surgeons, Seattle, the BA, October, 1998.
33) Brayda-Bruno M, Cinnella P: Posterior Endoscopic Discectomy and other procedures. Eur Spine J 2000; 9(suppl):S24-S29.
74) Boos's book: spinal disorders: fundamentals of dx and tx.
88) Schick U, Dohnert J, et al. “microendoscopic lumbar discectomy versus open discectomy: an intraoperative EMG study." Eur Spine J 2002; 1:20-6
110) Breasted JH (1930) Edwin Smith Surgical Papyrus, in Facsimile and Hieroglyphic Transliteration and with Translation and Commentary, 2 vols. Chicago: University of Chicago Oriental Publications.
111) Ohnmeiss DD, et al. "Degree of disc disruption and lower extremity pain" Spine 1997; 22(14):1600-1605
112) Ohnmeiss DD, et al. "Relation between pain location and disc pathology: a study of pain drawings and CT/discography." Clin J Pain 1999;15:210-7.
114) 14) Herkowitz HN, Dvorak K, Bell G, et al. "The Lumbar Spine-3rd edition." Lippincott Williams & Wilkins 2004; Philadelphia, PA
153) McCulloch JA (1996) Focus issure on lumbar disc herniation: macro-and microdiscectomy." Spine 21:45S-56S.
