Disc Volume Reduction Techniques
Chymopapain | Percutaneous Lumbar Discectomy | DeKompressor System | Nucleoplasty | Laser Discectomy | Research
 There is a "surgical shortcoming" to fill: we need a surgical treatment for symptomatic small contained disc herniations, which are typically refractory (don't respond well) to conservative care and do not respond well to open discectomy, microdiscectomy [53, 54] or even fusion [71-73, 55, 56, ]. Introducing the Disc Volume Reduction Surgical Techniques:
There is a "surgical shortcoming" to fill: we need a surgical treatment for symptomatic small contained disc herniations, which are typically refractory (don't respond well) to conservative care and do not respond well to open discectomy, microdiscectomy [53, 54] or even fusion [71-73, 55, 56, ]. Introducing the Disc Volume Reduction Surgical Techniques:
In hope of satisfying this need, surgeons and researches created a class of techniques that I like to call disc volume reduction techniques (DVRTs). Although they all use different twists on similar technology, DVRTs share one commonality: they are all performed without the use of scalpel or incision. Instead, a large hollow needed (cannula) is inserted through the skin, muscles, and connective tissue of the low back and into the damaged disk. Then different "flavors" of instruments (probes) are advanced through the cannula and into the center of the disc. All of these instruments also have one commonality: they are designed to remove nucleus pulposus tissue from inside the disc. This "volume reduction" ostensibly causes a retraction (or sucking in) or inward collapse of the small herniation, which in turn removes pressure from the nerve root(s) and dura of the thecal sac, as well as, diminishes the intradiscal pressure. This pressure reduction is thought to diminish the stimulation/irritation of sinuvertebral nerve endings in the posterior one third of the disc thereby reducing patient pain.
The beauty of these techniques, unlike traditional open discectomy/microdiscectomy, is that they do not enter the epidural space / vertebral canal, and do not call for the destruction of ligamentum flavum or any part of the posterior arch. Although these "minimally invasive procedures" sound good on paper, there is definite controversy as to whether or not they actually work.
The biggest criticism of these DVRTs is this: in order to fix the small disc herniation, the procedure requires a puncturing of the disc on the opposite side of the herniation. This is not a good thing! For we know from the sheep studies of the 1990s, as well as recent human-based investigations [12] that poking the hole in any part of the disc will not only cause accelerated degeneration and that disc, but will also significantly increase the chance of a developing a symptomatic and disabling disc herniation. [12]
Next I will cover (in chronological order) the more common DVRTs in hopes of giving you a better understanding of just how these treatment interventions are supposed to work.
Chymopapain Chemonucleolysis:
In 1963, after obtaining permission from the FDA, Lyman W. Smith performed the first human chymopapain chemonucleolysis by injecting chymopapain (the major proteolytic enzyme of papaya) into the center (the nucleus pulposus) of a herniated disc. This enzyme has an affinity (likes) for the high proteoglycan content of the nucleus pulposus and enzymatically destroys it. Because the annulus fibrosis has a much lower proteoglycan content than the nucleus pulposus, the annulus is ostensibly spared from destruction. Smith named this procedure chemonucleolysis [300].
How is destroying the center of the disc supposed to fix a posterolateral herniation, which is on the outside of the disc? As mentioned in the opening paragraphs, this destruction of nucleus pulposus will lead to a reduction in disc volume, which in turn reduces the intradiscal pressure. This pressure reduction then is supposed to "suck" the small herniation back into the disc from which it came from and thereby relieve any nerve root compression/irritation that this herniation was causing. The decreased intra-discal pressure will also relieve some of the irritating pressure that builds up within the annular tear and thereby decrease the lower back pain associated with the small disc herniations.
Although the results of early investigations into this new procedure were favorable (82% of the patients in one study achieved a "satisfactory" result), it soon became apparent that a small percentage of the patients were suffering serious adverse reactions to the enzyme. More specifically, in one study 0.06% of the patients undergoing the procedure suffered serious anaphylactic reactions (allergic reactions) to the papaya enzyme [303]. And if that wasn't bad enough, even more serious complications occurred when it became apparent that the Papaya enzyme, in some patients, was leaking out the back of the disc and destroying the adjacent nerve roots in cauda equina, which resulted in patient paralysis (transverse myelitis). [74, 75] Because of the foregoing reported complications as well as a controversial double-blind study by Cloud et al (1976), the US FDA banned chemonucleolysis with chymopapain in 1975.
Notwithstanding the US ban, research continued demonstrating the efficacy of this procedure on a very select group of patients—it is still performed in other parts of the world to this day [66]. In fact, with regard to chemonucleolysis with chymopapain, famed researcher and surgeon, Franco Postacchini stated, "Of all the percutaneous procedures, nucleolysis [via chymopapain] is that which provides the highest rate of satisfactory results," however, "compared with the other percutaneous procedures, chemonucleolysis implies a higher risk of complications, particularly of a serious type."[952].
Despite the bad reputation that chemonucleolysis has gotten in the United States, it remains the only minimally invasive procedure shown to be effective in prospective randomized studies. Moreover, a meta-analysis showed that chymopapain was more effective than placebo [49].
Percutaneous Lumbar Discectomy: (aka: Percutaneous Nucleotomy)
 Percutaneous Lumbar Discectomy is a minimally invasive, disc volume reduction procedure developed in the late 1970s for the treatment of small contained disc herniations [301, 302], which historically respond poorly to traditional open discectomy/microdiscectomy [12, 13].
Percutaneous Lumbar Discectomy is a minimally invasive, disc volume reduction procedure developed in the late 1970s for the treatment of small contained disc herniations [301, 302], which historically respond poorly to traditional open discectomy/microdiscectomy [12, 13].
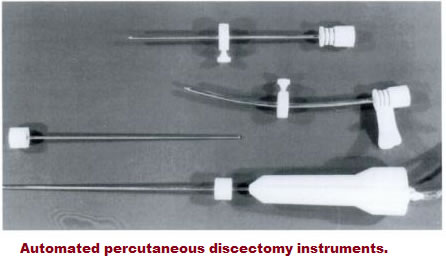
The initial, manual, versions of this technique were crude and afforded higher than desired complication rates. However, in the early 1980s Onik revamped the procedure and equipment into a methodology that continues to be in use to this very day [63-65]. Among other things, Onik's equipment was much smaller and less innocuous than those used by other surgeons for manual percutaneous nucleotomy. The technique quickly became very popular to to its technical simplicity and the high rate of patient satisfaction initially reported.
There were two probe designs that evolved with the passage of time: the first was called the Nucleotome aspiration probe (Clarus Medical), which is used in a procedure called automated percutaneous lumbar discectomy (APLD). This form of percutaneous lumbar discectomy is still the most widely performed lumbar minimally invasive procedure to date [60]. A second version, called the DeKompressor probe (Stryker medical), will be discussed later.
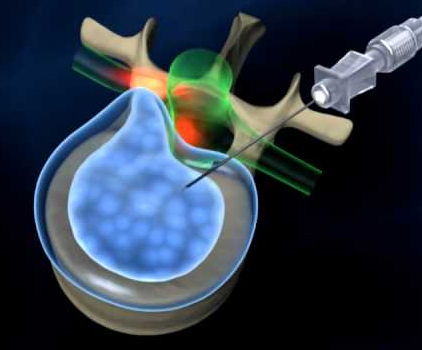
How does it work? This outpatient procedure, which is performed under local anesthesia, begins with the fluoroscopically-guided placement of a placing a guide needle / hollow cannula through the tissue of the lower back onto the posterolateral aspect of the disc. Next an annulus-cutting instrument (called a trephine) is pushed into the cannulus and is used to cut a 8-mm deep hole in the outer annulus. Then a special instrument called a probe (the nucleotome) is placed through the cannula and into the center of the disc (nucleus pulposus). This probe is then activated so that it removes nucleus pulposus by way of a suck-and-cut processes. The doctor must maneuver the Nucleotome in all regions of the nucleus in order to extract the necessary volume of nuclear tissue to get a reduction in disc volume / disc pressure. Aspirated nuclear material can then be collected in a bottle for study.
The beauty of this system is that the proteoglycans-rich nucleus pulposus is loose enough to be pulled into the probe; whereas, the collagenous annulus fibrosis is not, thereby protecting the annulus from being cut up. Because of the redesign, a very small cannula could now be used (2.8 mm), which mitigates the chances of injury to the annulus, blood vessels and nerves, as well as reduces the occurrence of epidural fibrosis and discitis [156, 308].
The goal of APLD is to reduce the "volume" of nucleus pulposus by approximately 3 grams [17-19, 126]. And because a contained disc herniation is still considered a hydraulic system (nothing leaking), a small reduction in volume leads to a large reduction in intradiscal pressure in accord with the laws of physics. As discussed previously, this intradiscal pressure loss does two things: (1) it will suck the herniated portion of the disc back into the center from which it came, thereby reducing any nerve root /thecal sac compression, and (2) it will reduce pressure-irritation upon the sensitive, pain-carrying, nerve endings of the sinuvertebral nerve, which of course are found in the outer one third of the posterolateral annulus fibrosis.
Candidates: The best candidates for this procedure are those of whom suffer a small contained disc herniation at a single level that does not contain a full thickness annular tear (so discography will have to be performed in order to assess the flavor of tear). The degree of disc degeneration should be minimal without a significant loss of disc height. With regard to symptomatology, it is better if the patient has leg pain (sciatica) greater than low back pain [60, 61]. Furthermore, this procedure is likely to fail in patients who have disc extrusions (aka, non-contained herniations) or sequestrations [62].
The forthcoming images depict a small contained broad based disc protrusion (left), which was completely reduced (right) following automated percutaneous lumbar discectomy (APLD).
The Research: Does this procedure work?
In 2009, a group of highly respected researchers (Manchikanti, Hirsch, and Singh) published the results of their evidence-based systematic review of previously published APLD studies [65]. More specifically, only studies of high scientific quality were reviewed. Of the two randomized controlled trials that were allowed into the investigation, APLD performed miserably as it was demonstrated to be not nearly as effective as chemonucleolysis using chymopapain [951] or traditional microdiscectomy [953]. Observational studies, however, described a more favorable outcome, although many would argue that randomized controlled trials are much more powerful than observational studies.
The bottom line of this systematic review was that there was what I will call middle-of-the-road evidence to support the efficacy (whether or not the damn thing worked) of APLD as a treatment intervention for small contained disc herniation [65]. [Read the whole story of this investigation here].
What is it? Onik’s automated percutaneous lumbar discectomy laid the foundation for the next twist on the minimally invasive bandwagon: the DeKompressor system. [306-308].
The DeKompressor™ Percutaneous Discectomy Probe is a patented probe that is intended for use during percutaneous lumbar, thoracic and cervical discectomy (PLD) procedures. The procedure is performed in the very similar manner as was described for the Nucleotome probe [here], and overall it is not much different than APLD [309]. However, unlike its predecessor, this probe removes a predetermined amount of disc material, which, as before, decreases the volume of the nucleus pulposus, which in turn leads to the retraction of the contained herniation and diminishes pressure on the sensitive, pain-carrying nerve fibers/receptors (sinuvertebral nerves) of the posterolateral annulus fibrosis of the disc. Among the claimed major advantages of this system, is the fact it uses an even smaller diameter cannula (1.5 mm {17G} or 1.0 mm {19}) that serves as a workspace/canal for tissue removal. One of the touted benefits of this procedure is that, because of the small cannula , it minimizes the risk of injury to disc during insertion, as well as decreases the chances for the development of epidural fibrosis [308]. Another advantage is the fact it removes disc material in a fashion that can be quantified and later, if so desired, examined histologically.
Does it work? In 2009, Singh et al. published the results of their systematic review of the DeKompressor system [309]. After reviewing the medical literature, only two articles had sufficient quality for inclusion into the study (both rated 52/100 on the AHRQ methodological assessment tool). To make things even worse, there were no randomized controlled trials identified. The researchers combined the results of the two observational studies for analysis. With regard to the level of evidence available to support the procedure’s efficacy, the DeKompressor system received "Level III for short-term and long-term relief of back and leg pain” via the USPSTF criteria [310]. Puyatt et al’s criteria [311] was used to generate a overall recommendation for the procedures efficacy: it was given a 2C/very weak rating. *The former and latter ratings were both the lowest available on the respective scales. So the answer to the original question is that based upon the current available studies and ratings, the DeKompressor system does not work as well as APLD (this had a Level II-2 rating), laser discectomy (this also had a Level II-2 rating) or nucleoplasty (this also had a Level II-2 rating). In conclusion, the authors opined, "The DeKompressor may be considered prior to open discectomy for patients with leg pain and a contained disc herniation." They also stated that it was relatively safe and destroys a minimal amount of tissue, which should mitigate disc height loss. They also state, "Automated percutaneous lumbar discectomy and laser discectomy have been shown to have better evidence with extensive experience [312, 313]. In all fairness, however, the poor ratings for DeKompressor were mostly due to the scarcity of properly designed observational studies and an absence of randomized controlled studies, so the opinions of these authors must be taken with a grain of salt – perhaps the jury is still out on this procedure.
Nucleoplasty:
 Percutaneous Disc Decompression using Coblation technology™ (aka Nucleoplasty) was approved by the FDA in year 2000 and has gained immediate popularity among surgeons (46, 41, 47). In fact, within two short years of its FDA approval, approximately 8000 patients had undergone the treatment (16).
Percutaneous Disc Decompression using Coblation technology™ (aka Nucleoplasty) was approved by the FDA in year 2000 and has gained immediate popularity among surgeons (46, 41, 47). In fact, within two short years of its FDA approval, approximately 8000 patients had undergone the treatment (16).
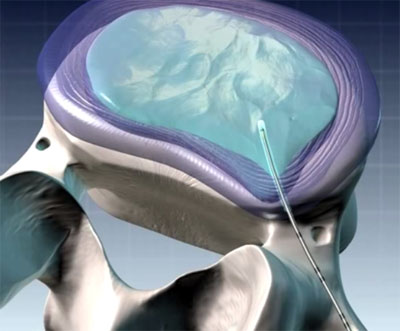
How does it work? This technique uses radiofrequency energy to carve small channels within the nucleus pulposus, which in turn causes a reduction in nuclear volume (41). These channels are then thermally treated in order to produce a zone of thermal coagulation, which in turn, ostensibly, decreases the volume of the disc. It is this volume decrease that (here we go again, same old story) leads to retraction of the herniation as well as pressure relief of the sensitive sinuvertebral nerve receptors. So you could say nucleoplasty combines coagulation and tissue ablation (the ablation is the patented parts of coblation technology) in order to affect a change in the intradiscal pressure.
Does it work? During the 12 years since its FDA approval, the efficacy of the procedure remains controversial, notwithstanding the increasing utilization of the procedure. For example, Gibson and Waddell (two extremely pessimistic, yet world-renowned spinal researchers) stated that all minimally invasive decompression techniques, including coblation therapy "should be regarded as research techniques"(40). To make things even bleaker, The Centers for Medicare and Medicaid Services (CMS) issued a non-certification for all of these minimally invasive disc decompression procedures, including nucleoplasty (48).
But to scientifically answer the question of whether or not it works, we turn to another systematic review of only the most scientifically based research papers. More specifically, in 2010 Gerges et al published the results of their investigation into the efficacy of nucleoplasty [102]. You can review the entire investigation here, but the bottom line was that there only slightly less than middle-of-the-road evidence was available to support its efficacy (i.e., there was a 1C Strong recommendation for its efficacy based on low-quality evidence). In other words, there is not much evidence to support that this works.
Percutaneous Laser Lumbar Discectomy:
In 1986, P.W. Ascher and Choy, first used laser energy to vaporize the nucleus pulposus in order to reduce discal volume, in order to retract small contained disc herniations. The beauty of this procedure was that it was performed through an even smaller channel—i.e., an 18 gauge needle—which was placed percutaneously into the lumbar disc using a posterolateral approach [68]. Since its introduction, however, concerns have been raised with regard to end plate injury, as well as its poor performance in randomized controlled trials, which showed chemonucleolysis more effective [69].
The obvious benefit of this procedure is that since it is carried out through such a small needle, it does not inflict much damage on to the annulus fibrosis. Furthermore, it greatly reduces epidural fibrosis and other complications because of its small size – it is truly minimally invasive.
But does it work? What does the research say? To answer this question, we turn to the familiar trio: Manchikanti, Hirsch, and Singh who published a systematic review of all of the published research papers on this topic [70]. As usual, only the most scientific papers were allowed in for consideration. The bottom line of their investigation [you can my review of their paper here] demonstrated, once again, middle-of-the-road evidence in support of laser lumbar discectomy. More specifically, there was a 1C / strong recommendation given based on low to very low quality evidence.
Ozone Therapy: Coming soon.
Endoscopic Discectomy:
In 1988, Kambin published the first endoscopic view of a herniated lumbar disc, Which was subsequently removed via endoscopic discectomy. This type of procedure is not a disc volume reduction technique, but a real direct excision form of discectomy (it physically removes chunks of herniated nuclear material just like open discectomy or microdiscectomy). In a later study (after further refinement of the technique), Kambin et al reported a favorable outcome – similar to success rates boasted by open discectomy – in 87% of a select group of patients [76]. Yeung et al. [77]also reported on the outcome of endoscopic discectomy. In this retrospective study of 307 patients who underwent percutaneous posterolateral nucleotomy for lumbar disc herniations, it was demonstrated that at the one year time point, 90.7% of the patients were satisfied with the procedure and would repeat the procedure under the same circumstances. He concluded that percutaneous posterolateral in this topic discectomy has comparable results to open microdiscectomy. [my review].
In 2005, Ruetten et al. published the results of their investigation into an endoscopic discectomy technique that used an extreme lateral approach for herniations inside the spinal canal. More specifically, they reported on the outcome of 463 patients who had hernia exclusion via the extreme lateral approach. At the outcome time point, 81% of the patients had a complete resolution of their leg pain, which is certainly comparable with open discectomy/microdiscectomy. [78]
REFERENCES:
1) Milette PC, et al. “Radiating Pain to the Lower Extremities Caused by Lumbar Disk Rupture without Spinal Nerve Root Involvement.” AJNR Am J Neuroradiol 1995; 16:1605-16132) Ohnmeiss DD, et al "Degree of disc disruption and lower extremity pain" Spine - 1997; 22(14):1600-1665 (also in several other journals in 1999)
3) Marshall LL, et al. “Chemical irritation of nerve root in disc prolapse.” Lancet 1973; 2:320
4) Marshall LL, et al. “Chemical Radiculitis: A clinical, physiological and immunological study. Clin Orthop 129:61-67, 1977
5) Saal JA, Saal JS, Richard JH. The natural history of lumbar intervertebral disc extrusion treated nonoperatively. Spine
1990,15:683–6.
6) Eiichi Takada and Masaya Takahashi et al. "Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome. "Journal of Orthopaedic Surgery 2001, 9(1): 1–7
7) Goupille et al. "Percutaneous Laser Disc Decompression for the treatment of Lumbar disc herniation." Semin Arthritis Rheum. 2007 Mar 13; (Epub ahead of print).
8) Anderson GBJ. The Epidemiology of Spinal Disorders. In: Frymoyer JW, ed. The Adult Spin. New York: Raven press; 1997
9) Van de Velden J, de Bakker DH. Basisrapport: morbiditeit in de huisartsenpraktijk. Utrecht: Nivel;1990
10) Carragee EJ, et al. "Can MR scanning in patients with sciatica predict failure of open limited discectomy? Proceeding of the international Society for the study of lumbar spine (ISSLS) Scotland, June 2001
11) Peng B, Wenwen W, et al. “Chemical Radiculitis." (2007) Pain 127(11-16)
12) Carragee EJ, Don AS, Hurwitz DC, et al. "2009 ISSLS Winner: does discography cause accelerated progression of degeneration changes in the lumbar disc? A 10-year matched cohort study. Spine 2009; 34 (21): 2338-2345.
13) Atlas SJ, et al. "Surgical & nonsurgical management of sciatica secondary to a lumbar disc herniation: Five year outcomes from the Maine Lumbar Spine Study." Spine - 2001; 26(10):1179-1187: AND : Atlas SJ, Deyo RA, et al. 'Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study.' Spine. 2005 Apr 15;30(8):927-35 [here]
14) Brouwer PA, et al. "effectiveness of percutaneous laser disc decompression versus conventional open discectomy in the treatment of lumbar disc herniation; design of a prospective randomized controlled trial." 2009; BMC Musculoskeletal Disorders 10:49
15) Schenk B, et al (2006) Percutaneous Laser Discectomy: A Review of the Literature. AJNR; January 2006: 27; 232-235 [here]
16) Singh V, et al "Percutaneous Disc Decompression using coblation (Nucleoplasty) In the Treatment of Chronic Discogenic Pain." 2002 Pain Physician, Volume 5, Number 3, pp 250-259 ASIPP.
17) Waddell G. "A new clinical model for the treatment of low back pain." (1987) Spine; 12:632-44
18) Croft PR et al. "Outcome of low back pain in general practice prospective study." (1998) BMJ; 316:1356-9.
19) Schwarzer AC, Aprill CN, Derby R, Bogduk N, Kine G. "The prevalence and clinical features of internal distant instruction in patients with chronic low back pain." (1995) Spine; 20(17):1878-83.
20) Manninen P, et al. "Incidence and risk factors of low-back pain in middle aged farmers." (1995) Occupation Med (Oxf; 45:141-146)
21) Merskey H, Bogduk N. “Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms.” Seattle: IASP Press, 1994:180-1
22) Carragee EJ, et al "Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment types and annular competence" J Bone Joint Surg Am - 2003; 85(1):102-108
23) Karppinen J. et al. “Severity of Symptoms and Signs in Relation to Magnetic Resonance Imaging Findings Among Sciatic Patients.” Spine 2001;26(7):E149-E154 [here's my review].
24) Modic MT, et al. “Contrast-enhanced MR imaging in acute lumbar radiculopathy: a pilot study of the natural history.” Radiology 1995 ;195:429-35
25) Jensen MC, et al. “MRI imaging of the lumbar spine in people without back pain.” N Engl J Med – 1994; 331:369-373
26) Boden SD et al. “Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects: A prospective investigation.” J Bone Joint Surg Am 1990; 72A:403-408
27) Lawrence RC, et al. "estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States." (1998) Arthritis Rheum; 41:778-799.
28) Gureje O, et al. "Persistent pain and well-being: a World Health Organization study of primary care." (1998); 280:147-151
29) Cassidy D, et al. "The Scandinavian health and back pain survey." (1998); 23:1860-67
30) Manchikanti L. "Epidemiology of Low Back Pain." (2000); 3:167-192
31) Walker BF. "The Prevalence of Low Back Pain: (2000); J Spinal Discord; (13:205-217
32) Kuslich SD, et al. "The Tissue Origin of Low Back Pain and Sciatica: A report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia." Orthop Clinics North Am 1991 ;22 (2):181-187
33) Manchikanti L, Derby R, Hirsch JA, et al. "a systematic review of mechanical disc decompression with nucleoplasty." Pain Physician 2009; 12:561-572
34) Chen YC et al. "intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers." Spine 2003; 28:661-665.
35) Kambin P, et al. "percutaneous posterolateral discectomy. Anatomy and mechanism." Clin Orthop Relat Res 1987; 223:145-154.
36) Kambin P, el al. "Percutaneous lumbar discectomy. Review of 100 patients and current practice." Clin Orthop Relat Res 1989: 238:24-34
37) Karasek M, Bogduk N. "12 month follow-up of controlled trial of intradiscal thermal annuloplasty (IDET) four back pain do to internal disc disruption." spine 2000; 25:2601-2607.
38) Nerubay J, et al. "percutaneous laser nucleolysis of the intervertebral disc. An experimental study." Clin Orthop Relat Res 1997; 337:42-44.
39) Sasaki M, et al. "effects of chondroitinase ACB on intradiscal pressure in sheep: an invivo study." Spine 2001; 26:463-468.
40) Gibson JNA, Waddell G. "surgical interventions for lumbar disc prolapse." Cochrane Database Syst Rev 2009; 1:CD001350.
41) Chen YC, et al. "intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers." Spine 2003; 28:661-665.
42) Mixter W, Barr J. rupture of the intervertebral disc with involvement of the spinal canal." N Engl J Med 1934; 211:210-215.
43) Smith L. "enzymatic dissolution of the nucleus pulposus in humans." JAMA 1964; 187:137-140.
44) Hijikata S. "percutaneous Nucleotomy: a method of percutaneous nuclear extraction." J Toden Hospital 1975; 5:39-44.
45) Onik G, et al. "percutaneous lumbar discectomy using a new aspiration probe." AJNR 1985; 6:290-293.
46) Derby R, Baker RM, Lee CH. "evidence-informed management of chronic low back pain with minimally invasive nuclear decompression." Spine J 2008;8:150-159
47) Chen YC, et al. "histologic findings of disc, end-plate and neural elements after a collation of nucleus pulposus: an experimental nucleoplasty study." Spine J 2003; 3:466-470.
48) Phurrough S, et al. "Decision Memo for Thermal Intradiscal Procedures. 2008 [cited September 30, 2008]. www.cms.hhs.gov/mcd/viewdecisionmemo.asp?from2=viewdecisionmemo.asp&id=215&
49) Gibson JN, Grant IC, Waddell G. "the Cochrane review of surgery for lumbar disc prolapse and degenerative lumbar spondylolisthesis." Spine 1999; 24:1820-1832.
50) Ng LC, Sell P. 'Predictive value of the duration of sciatica for lumbar discectomy. A prospective cohort study.'J Bone Joint Surg Br. 2004 May;86(4):546-9 " Patients with an uncontained herniated disc had a shorter duration of symptoms and a better functional outcome than those with a contained herniation."
51) Karppinen J. et al. “Severity of Symptoms and Signs in Relation to Magnetic Resonance Imaging Findings Among Sciatic Patients.” Spine 2001 ;26(7):E149-E154
52) Modic MT, et al. “Contrast-enhanced MR imaging in acute lumbar radiculopathy: a pilot study of the natural history.” Radiology 1995 ;195:429-35.
53) Carragee EJ, et al "Clinical outcomes after lumbar discectomy for sciatica: The effects of fragment types and annular competence" J Bone Joint Surg Am - 2003; 85(1):102-108.
54) Dewing CB, et al. "the outcome of lumbar microdiscectomy in a young, active population: correlation by herniation type and level." Spine 2008; 33:33-38.
55) Brox JI, et al. “randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercise in patients with chronic low back pain and disc degeneration." Spine 2003; 28:1913-1921.
56) Ekman P, et al. “long-term effect of posterolateral fusion in adult isthmic spondylolisthesis: a randomized control study." Spine J 5:36-44.
57) Hoppenfeld S. “percutaneous removal of herniated lumbar discs: 50 cases with 10 year follow-up periods.” Clin Orthop 1989;238:92-106.
58) Kambin P, Schaffer JL. “Percutaneous lumbar discectomy: review of 100 patients and current practice." Clin Orthop 1989; 289:24-34.
59) Onik G, Helms CA. “Automated percutaneous lumbar discectomy." AJR 1991; 156: 531-538.
60) Vaccaro AR, Bono CM. “minimally invasive spine surgery.” (2007) In: Informa Healthcare USA, Inc. 52 Vanderbilt Ave., New York, NY 10017.
61) Singh V, Manchikanti L, Helm S, Hirsch et al. “Percutaneous Lumbar laser Disc Decompression: a Systematic Review of Current Evidence." Pain physician 2009; 12:573-588.
62) Marron JC, Onik G, Sternau L. “percutaneous automated discectomy: a new approach to lumbar spine." Clin Orthoop 1989; 238:64-70.
63) Onik G, Helms C, et al. "percutaneous lumbar discectomy using a new aspiration probe." AJNR 1985; 6:290-293.
64) Onik G, Helms CA et al. “percutaneous lumbar discectomy using a new aspiration probe: porcine and cadaver model. Radiology 1985; 155:251-252.
65) Hirsch JA, Singh V, Manchikanti L, et al. “Automated Percutaneous Lumbar Discectomy For the Contained Herniated Lumbar Disc A Systematic Assessment of Evidence." Pain Physician 2009; 12:601-620.
66) Wittenberg RH, et al. “five-year results from chemonucleolysis with chymopapain or collagenase: a prospective randomized study." Spine 2001; 26(17):1835-41 German study.
68) Choy DS, Case RB, et al. “Percutaneous laser nucleolysis of lumbar discs.” N Engl J Med 1987; 317:771-772.
69) Rheinhard SWR, Kraemer J. “chemonucleolysis versus laser decompression: a prospective randomized trial.” J Bone Joint Surg Br 1997; 79:247.
70) Singh V, Manchikanti L, Helm S, Hirsch et al. “Percutaneous Lumbar laser Disc Decompression: a Systematic Review of Current Evidence." Pain physician 2009; 12:573-588.
71) Slosar PJ, Reynolds, JB, et al. "Patient satisfaction after circumferential lumbar fusion." Spine 2000; 25(6):722-726.
72) Wetzel FT, LaRocca SH, et al. "The treatment of lumbar spinal pain syndromes diagnosed by discography: Lumbar arthrodesis." Spine 1994;19:792-800.
73) Zdeblick TA. A prospective, randomized study of lumbar fusions: preliminary results. Spine 1993;18:983-991.
74) Muralikuttan KP, Hamilton A, et al. "a prospective randomized controlled trial of chemonucleolysis and conventional disc surgery and a single level lumbar disc herniations." Spine 1992; 17:381-387.
75) Brown MD. "Update and chemonucleolysis." Spine 1996; 21:62S-68S.
76) Kambin P, Zhou L. "history and current status of percutaneous arthroscopic disc surgery." Spine 1996; 21:57S-61S.
77) Yeung AT, Tsou PM. "posterolateral endoscopic excision for lumbar disc herniations: surgical technique, outcome, and complications in 307 consecutive cases." Spine 2002; 27:722-731.
78) Ruetten S, Komp M, Godolias G. "an extreme lateral access for the surgery of lumbar disc herniations inside the spinal canal using full endoscopic uniport transforaminally approach technique and prospective results of 463 patients."Spine 2005; 30:2570 – 2578.
99) Toyone T, Tanaka T, et al. 'Low-back pain following surgery for lumbar disc herniation. A prospective study.' J Bone Joint Surg Am. 2004 May;86-A(5):893-6 "Excision of a herniated disc for relief of sciatica provided rapid relief of sciatica and low-back pain. The findings of the present small study suggest that lumbar disc herniation might be a possible cause of low-back pain."
100) Deyo RA, Weinstein JN. Low back pain. N Engl J Med.
101) Weinstein JN, et al. "Surgical vs nonoperative treatment for lumbar disc herniation: The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA 2006; 296:2441-2450.
102) Gerges FJ, Lipsitz SR, Nedeljkovic SS. “A Systematic Review on the Effectiveness of the Nucleoplasty Procedure for Discogenic Pain." Pain Physician 2010;13: 117-132.
117) Boswell MV, Singh V, Manchikanti L, et al. "Interventional techniques: Evidence-based practice guidelines in the management of chronic spinal pain." Pain Physician 2007; 10:7-111.
118) Manchikanti L, et al. " Physician payment 2008 for interventionalists: current state of health care policy." Pain Physician 2007; 10:607-626.
119) Manchikanti L, Singh V, Hirsch JA, et al. "Analysis of growth in interventional techniques in managing chronic pain in Medicare population: a 10-year evaluation from 1997 to 2006. Pain Physician 2009; 12:9-34.
149) Manchikanti L, Derby R, Helm S, Hirsch JA, et al. “a systematic review of mechanical lumbar disc decompression with nucleoplasty." Pain physician That 2009; 12:561-572.
150) Singh VJ, et al. “Percutaneous disc decompression using Coblation (nucleoplasty) in the treatment of chronic discogenic pain." (2002) Pain Physician; 5(3): 250-59.
151) Derby R, et al. "evidence informed management of chronic low back pain with minimally invasive nuclear decompression." Spine J 2008; 8:150-151.
125) Mixter WJ, Barr JS. “Rupture of the intervertebral disc with involvement of the spinal canal.” N Engl J Med 1934; 211:210-5
170) Karppinen J, et al. “Severity of Symptoms and Signs in Relation to Magnetic Resonance Imaging Findings Among Sciatic Patients.” Spine 2001; 26:E149-E154
290) Kortelainen P, et al. “Symptoms and signs of sciatic and their relation to the location of the lumbar disc herniation.” Spine – 1985; 10:88-92
300) Widell EH, Vanesian R. “chymopapain chemonucleolysis.” Calif Med. 1973; 118(3): 35-36.
301) Kambin P, Gellman H, “percutaneous lateral discectomy of the lumbar spine: a preliminary report." Clin Orthoop 1983; 174:127-132.
302) Hijikata S. “percutaneous nucleotomy. A new concept technique and 12 years experience." Clin Orthoop Relat Res 1989; 238:9-23.
303) Javid MJ et al. “safety and efficacy of chymopapain in herniated nucleus pulposus with sciatica." JAMA 1983; 249:2489-2494.
304) Onik G, et al. “percutaneous lumbar discectomy using a new aspiration probe." AJR 1985; 144:1137 – 1140.
305) Krugluger J, Knahr K. “chemonucleolysis and automated percutaneous discectomy – a prospective randomized comparison." Int Orthop 2000;24(3):167-9.
306) Alo KM et al. “percutaneous lumbar discectomy: clinical response in an initial cohort of 50 consecutive patients with chronic radicular pain." Pain Pract 2004; 4:19-29.
307) Alo KM, et al. “percutaneous lumbar discectomy: one-year follow-up in an initial cohort of 50 consecutive patients with chronic radicular pain."Pain Pract 2005; 5:116-124.
308) Lierz P, et al. “percutaneous lumbar discectomy using the DeKompressor system under CT control.) Pain Pract 2009; 9:216-220.
309) Singh V, Manchikanti L, et al. “systematic review of percutaneous lumbar mechanical disc decompression utilizing DeKompressor." Pain Physician 2009; 12:589-599.
310) Berg AO Allan JD. “Introducing the third US preventative service task force." Am J Prev Med 2001; 20:S3-S4.
311) Guyatt G, et al. “grading strength recommendations and quality of evidence in clinical guidelines. Report from an American College of chest physicians task force." Chest 2006; 129:174-181.
312) Hirsch JA, et al. “automated percutaneous lumbar discectomy for the contained herniated lumbar disc: a systematic assessment of evidence." Pain physician 2009; 12:601-620.
313) Singh V, et al. “percutaneous lumbar laser disk decompression: a systematic review of current evidence." Pain physician 2009; 12:573-588.
314)*book reference: Onik GM, Helms CA, et al. “percutaneous lumbar discectomy using an aspiration probe." AJRN 1985; 6:290-293.
951) Chatterjee S, Foy PM, Findlay GF. “Reporting a controlled clinical trial comparing automated percutaneous lumbar discectomy and microdiscectomy in the treatment of contained lumbar disc herniation." Spine 1995; 20:734-738.
952) Postacchini Franco et al. In: " Lumbar disc herniation." 1999 Springer-Verlag/Wien; New York.
953) Revel M, et al. “automated percutaneous lumbar discectomy versus chemonucleolysis in the treatment of sciatica: a randomized multi-center trial." Spine 1993; 18:1-7.
